2021 MIPS Final Rule: Key Highlights & How to Maximize Your Quality Measures Score with CheckinAsyst
With healthcare practices continuing to forge ahead into the new financial year, preparing for the Merit-based Incentive Payment System (MIPS) reporting period is one of the key priorities.
On December 1, 2020, the Centers for Medicare and Medicaid Services (CMS) released the 2021 Final Rule for MIPS, one of the two tracks of the Quality Payment Program (QPP).
We bring you the main highlights of the Final Rule here. We’ll also discuss how practices can leverage CheckinAsyst to capture patient data and get the maximum score in the Quality category.
Key Takeaways
1. Performance Category Weight
The biggest change for the new rule in 2021 is the performance category weights. All the clinicians applying for an individual, group, or virtual MIPS scoring have to adjust their reporting based on the revised weight.
Note: This equates to the 2023 payment year.
- Quality: 40% decrease from last year)
- Cost: 20% (5% increase from last year)
- Promoting Interoperability: 25% (no change)
- Improvement Activities: 15% (no change)
When it comes to the performance threshold, physicians need to make every point in the above categories count as the performance threshold (minimum MIPS points required to avoid penalties) has been raised to 60 points. This means a 15-point increase in the threshold value from the previous year.
For the Quality Category:
CMS has introduced substantive changes to 113 existing quality measures. While 11 measures have been removed, two new quality measures have been added to the list. This includes:
- Hospital-Wide Readmission (HWR) Rate
- Risk-standardized complication rate (RSCR) following elective primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA)
For the Cost Category:
Apart from the 5% increase in weightage, the Cost category has minimal changes. CMS will include telehealth services directly applicable to existing episode-based cost measures and the Total Per Capita Cost (TPCC).
For the Improvement Activities Category:
There are no significant updates for the Improvement Activities category. CMS will modify two existing measures and remove an obsolete measure. Also, the COVID-19 clinical data reporting activity will continue with a slight modification to the activity description.
For the Promoting Interoperability Category:
In this category, CMS has decided to retain the Query of Prescription Drug Monitoring Program (PDMP) measure as optional. However, if utilized, you can earn 10 bonus points. An optional Health Information Exchange (HIE) bi-directional exchange measure has been added as an alternative reporting option to the measures related to the HIE objective. Also, Certified Electronic Health Record Technology (CEHRT) requirements are to be updated.
2. Payment Adjustment
In terms of payment adjustment, the 2021 rule has no changes. So, if you fall short of the threshold, you’ll receive a -9% penalty in your Medicare Part B payments of 2023, and if your points are above the minimum bar, you have an opportunity of receiving up to a +9% advantage.
Maximizing Your MIPS Quality Measures Score with CheckinAsyst
While the Quality category weightage may have dropped by five points, eligible physicians shouldn’t undermine its contribution to the Final Performance Score. To achieve a higher score, you have to focus on scoring the maximum allowable points in the Quality category.
However, collecting data for your quality measures is a burdensome program. As you need to report performance data for 70% of your patients, capturing the data can be challenging. Add to it the chaotic environment caused due to COVID-19, and this reporting year can be laborious for your staff.
CheckinAsyst ensures you do not miss out on any opportunity to collect Patient Reported Outcome (PRO) by making relevant questions mandatory during the intake process. Using the similar process, you have a fool-proof way to capture the required data for your quality measures exactly where you have your patients’ undivided attention –right at the point of check-in.
Automated Intake Workflows
Here’s how it works:
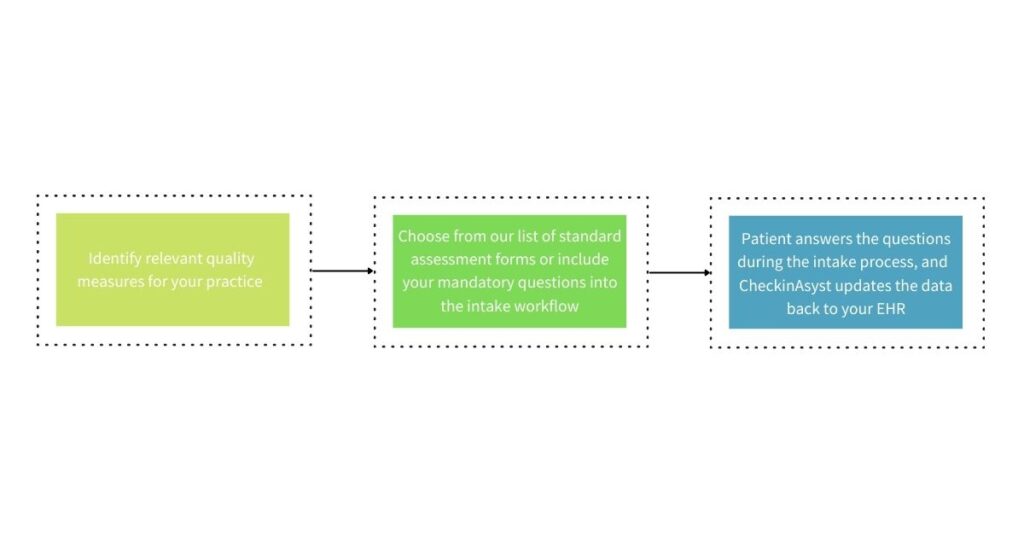
With a simple 3-step process, your practice can automate the data collection workflow. Also, by making it mandatory for your patients to complete these forms as part of the intake process, your chances of capturing data from maximum patients are much higher.
Eligible physicians can choose their preferred six quality measures and pick from our list of standard assessment forms based on their specialty. Once the information is captured, CheckinAsyst will automatically take the data back to your EHR, where you can use your reporting tool to track your progress.
How does this help your practice?
With an automated workflow for your MIPS Quality Measure reporting, your practice can see the below benefits:
Higher chances of collecting patient data using mandatory assessment forms
Minimal staff intervention as they needn’t follow up with the patients constantly
Ability to save both human effort and time using an automated workflow
Automated reports to analyze top-performing measures
Success Story
Tallahassee Neurological Clinic (TNC) provides neurology, neurosurgery, and pain management services for North Florida and South Georgia residents. TNC adopted CheckinAsyst for digitizing their intake workflow and incorporated questions related to their chosen Quality Measures right into the workflow. They selected the below measures that were relevant to their practice:
- Any falls in the past year (CMS 139)
- If the patient is a smoker (CMS 138)
- If the patient has had a Colonoscopy (CMS130)
- If the patient has had a Mammogram (CMS 125)
- If the patient has had a Pap Smear (CMS 124)
- Documentation of Current Medications (CMS 68)
TNC made the questions related to these measures mandatory within the check-in process and collected patient data seamlessly. TNC has been leveraging CheckinAsyst to capture MIPS Quality Measures and has been achieving the maximum allowable points under the Quality category since two years.
“I am happy to say we already achieved the highest allowable points this year for quality.”
Evie Van Rijs, Clinical Services Manager, Tallahassee Neurological Clinic
Next Steps
MIPS is here to stay and there is no debate that the program continues to get harder. Intelligent and automated workflows that allow you to capture relevant data at the point of service is a key driver for success in performing well under the Quality category.
Contact us to know more about how to automate your patient intake workflows to capture MIPS Quality measures data without compromising on patient experience and practice efficiency.







![Great [Patient] Expectations](https://www.healthasyst.com/checkinasyst/wp-content/uploads/2021/06/Great-Patient-Expectations-768x510.jpg)